“Respiratory syncytial virus was previously responsible for a large proportion of illnesses and deaths around the world. “I think this will change dramatically,” says Louis Pont, an infectious diseases pediatrician at University Medical Center Utrecht in the Netherlands. However, he warns that this positive development is unlikely to happen equally everywhere: costs and infrastructure problems will certainly delay some populations’ access to medicines in low- and middle-income countries. Even in wealthier parts of the world, the question arises as to how different prevention strategies can be used more safely and effectively.
The first attempt to develop a vaccine against the RSV virus Clinical testing began in the 1960s. That was less than a decade after scientists first isolated the pathogen from young children with severe pneumonia. But this approach proved disastrous, and even worsened the symptoms of the disease. “This has hampered efforts to find a successful vaccine for decades,” says Varga (see “Friendly Fire”). In the past 10 years, the development of RSV vaccines has accelerated again. Among other things, experts have identified the component of the virus that causes a strong immune reaction, which in turn can neutralize the infection and prevent it from becoming severe.
friendly fire
The ideal effect of a vaccine – which is rarely achieved in practice – is to protect the recipient 100% against all future encounters with the pathogen. The success of a vaccine can also be measured by whether it prevents serious diseases or reduces their transmission. However, the first vaccine against respiratory syncytial virus (RSV) did not exceed this threshold. Four clinical trials in the late 1960s were examples of a worst-case scenario, where vaccination caused a more severe course of the disease: in a study With 71 infants, 80% of the vaccinated children who became infected with RSV were hospitalized, compared with only 5% of the control group. Two of the vaccinated children who were treated in intensive care eventually died of infection.
This worrying finding was surprising for several reasons; Among other things, because the vaccine itself was ordinary. Respiratory syncytial virus particles are inactivated by treating them with formalin, an agent that chemically stabilizes proteins so that they can no longer carry out their intended biological function. This was combined with an immune stimulant made from aluminum salts called alum. This approach was standard in the 1960s. Both formalin inactivation and adjuvants are still used in some modern vaccines, according to Steven Varga, an immunologist at St. Jude Children’s Research Hospital in Memphis, Tennessee. For example, hepatitis B and pneumococcal alum vaccines are used, and inactivated polio vaccines are made from virus particles inactivated in formalin.
Experts were not able to clarify the factors that led to this negative scenario until after decades of investigations and discussions. “It was a coincidence of several events that led to the vaccine exacerbating the disease in children,” explains Varga. One of them: through treatment with formalin, the virus particles acquired a structure that stimulates the production of antibodies in the body, which bind well to viral proteins; However, they are unable to neutralize RSV infection. In fact, some studies suggest that they can accumulate as immune complexes in the lungs and trigger a harmful inflammatory response.
At the same time, the inactivated virus appears to hinder the formation of killer T cells, which normally destroy virus-infected cells in future encounters. This has left a crucial gap in the antiviral immune system. Instead, the vaccine elicited a strong response from a subset of helper T cells, which recruited a host of other immune cells during infection, which in turn could trigger a powerful and destructive inflammatory response in the lungs.
This is not a phenomenon unique to respiratory syncytial virus – similar problems occurred with formalin-inactivated measles vaccine in the same decade. However, formalin inactivation does not appear to be a problem with other vaccine preparations. Varga points out that both measles and respiratory syncytial virus belong to the paramyxovirus family. “I think it’s a common problem for this particular group of viruses,” he says.
Fortunately, subsequent cases of illness caused by the vaccine were extremely rare. According to Louis Pont, an infectious diseases pediatrician at the University Medical Center in Utrecht, the Netherlands, vaccine developers are now better able to intercept such effects before they occur in humans. “In the 1960s, we thought we could develop a vaccine against everything overnight,” Pont explains. “Preclinical and early clinical development is now more streamlined.”
Respiratory syncytial virus relies on a surface molecule known as a fusion protein (F) to attach to and invade host cells. Virologists quickly realized that this protein was a promising target for antibody-mediated immune attack. However, it comes in different forms. F alternates seamlessly between the “pre-merger” compact structure and the “post-merger” extended structure. The pre-fusion form, which makes it easier for the virus to penetrate the cell membrane, can be easily neutralized by antibody binding. For this reason, they are an excellent target for vaccines.

“Alcohol buff. Troublemaker. Introvert. Student. Social media lover. Web ninja. Bacon fan. Reader.”






More Stories
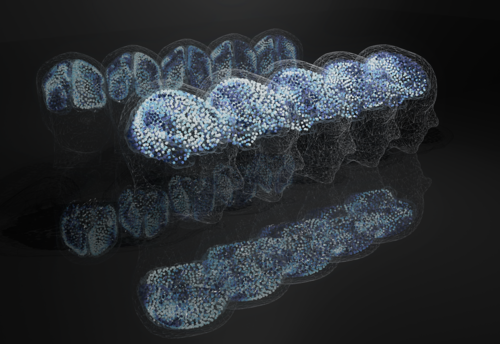
Researchers from Bosnia and Herzegovina develop theory about traveling waves of activity in the brain – News
Citizens’ help needed: Hedgehog and mole census campaign – Science
New vaccine against dengue » Latinapress News