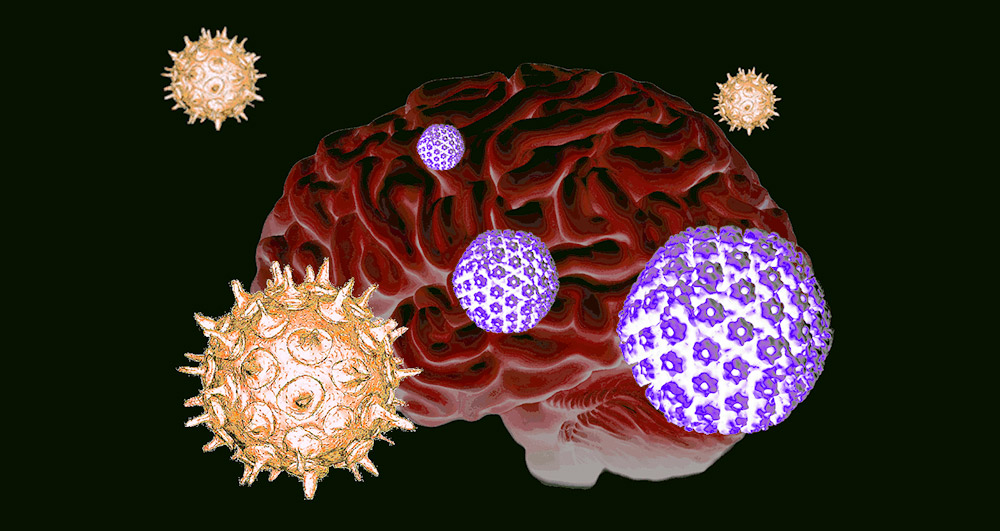
Viral double whammy: Anyone who has had cold sores and had chickenpox in the past can increase the risk of Alzheimer’s disease. Because when the viral pathogens of both diseases – the herpes simplex virus and the varicella-zoster virus – collect in the brain, it can lead to the formation of protein plaques typical of Alzheimer’s disease. A research team reports that the reason for this is most likely an inflammatory reaction that activates the dormant herpes virus.
Whether it’s cold sores, chickenpox, shingles, or Epstein Bar: Viral agents that cause these diseases all belong to the herpes viruses. A typical feature of these DNA viruses is their ability to be latent: after initial infection, they remain in the body forever and remain in a somewhat dormant state. Only when the immune system is weakened, the herpes viruses active again.
According to estimates by the World Health Organization, two-thirds of people carry the causative agent of cold sores, herpes simplex 1 (HSV-1). 95 percent of people have varicella zoster, which causes chickenpox and herpes zoster.
Alzheimer’s caused by herpes viruses?
It has long been suspected that herpes viruses also play a role in Alzheimer’s disease. Evidence for this is provided by the increased incidence of some herpes viruses in the brain deceased Alzheimer’s patients, but also laboratory experiments on tissue cultures of human brain cells. In this, a team led by Dana Karens of Tufts University in Massachusetts DiscoverInfection of these cultures with herpes virus can lead to increased formation of neurotransmitters and protein deposits typical of Alzheimer’s disease.
In another study, Kearns and her colleagues have now examined in more detail what’s behind it and when herpes viruses can cause Alzheimer’s symptoms in the brain. To do this, they grew 3D tissue cultures of neural stem cells, which consist of human neurons and helper cells, glial cells. They then infected these cell cultures with herpes simplex and/or varicella zoster.
Alzheimer’s disease plaques after double injury
It turns out that if brain cells were infected only with the shingles virus Varicella zoster, it could damage glial cells and release inflammatory messengers – but no Alzheimer’s plaques. However, this was different if the brain cells had previously been occultly infected with herpes simplex: the double infection reactivated dormant HSV-1 viruses and led to the rapid formation of misfolded amyloid beta and tau proteins – the characteristic plaques of Alzheimer’s disease.
As a result of this viral chain reaction, brain cells in the cultures become less active and eventually die. “Our results indicate that varicella infection causes inflammatory signals in the brain, which in turn wake up herpes simplex,” Kearns explains. This supports the indirect role of the chickenpox pathogen in Alzheimer’s dementia. At the same time, this may explain why latent herpes simplex infection alone does not appear to be sufficient to induce disease – the virus must be reactivated.
“It’s a double whammy of two viruses that are very common but often harmless when viewed alone. But when they do come together, it can cause problems,” explains Kearns.
The shingles vaccine may protect against
The fact that people vaccinated against chickenpox and shingles are less likely to develop Alzheimer’s also fits with the “partner” role of the chickenpox virus. They also have fewer cold sores on the lips. Kearns and her team attribute this to the fact that the “waking up” effect of inflammation caused by the varicella virus on the latent herpes infection then failed to appear. HSV-1 remains dormant and therefore its harmful effect cannot be detected.
However, whether the shingles vaccine, which is recommended for older adults anyway, can actually protect against Alzheimer’s disease or at least reduce the risk, needs to be closely examined. The researchers also acknowledge that HSV-1 Vren in the brain may also be reactivated by other influencing factors. “It is possible that other inflammatory events in the brain also lead to a resurgence of the herpes virus,” Kearns says. These include risk factors such as head trauma, obesity and alcohol consumption. (Journal of Alzheimer’s Disease, 2022; doi: 10.3233/JAD-220287)
Source: Tufts University

“Alcohol buff. Troublemaker. Introvert. Student. Social media lover. Web ninja. Bacon fan. Reader.”




More Stories
Huge radiation explosion from a magnetar – forschung.de
Principles and features of the folk nutritional principle
Science: The percentage of women in mint topics rises to a third